Important Update on Effective Mastitis Treatment Guidelines.
The Academy of Breastfeeding Medicine, a global organisation of dedicated healthcare professionals supporting breastfeeding, has recently released new mastitis guidelines. These guidelines acknowledge the limitations of traditional treatments, which could unintentionally worsen mastitis symptoms.
Mastitis is a common complication faced by breastfeeding women and often can contribute to choosing to end their breastfeeding journey early. Mastitis refers to the inflammation of the milk duct, often caused by the milk staying stagnant in the breast tissue or from a bacterial infection. The inflammation leads to various uncomfortable symptoms, ranging from pain and tenderness to fever and malaise.
There are two main types of mastitis: lactational mastitis and non-lactational mastitis. Lactational mastitis is commonly seen in breastfeeding individuals, while non-lactational mastitis can occur in those who are not breastfeeding, typically due to a bacterial infection. Throughout this blog we will be discussing lactational mastitis.
Factors for Lactation Mastitis:
- Bacterial Infection: One of the causes of mastitis is a bacterial infection, often stemming from cracked or damaged nipples. Bacteria can enter through these openings and cause inflammation.
- Milk Stagnation: When milk is not properly drained from the breast, it can lead to milk stasis, creating an ideal environment for bacterial growth. This often occurs due to poor breastfeeding techniques or infrequent feeding.
Symptoms of Mastitis:

- Swelling and redness of the breast
- Sore breast or tenderness
- Warmth to the touch
- Breast lumps
- Flu-Like Symptoms such as fever and chills
- Fatigue and malaise
- Body aches
What Are The New Mastitis Treatment Options?
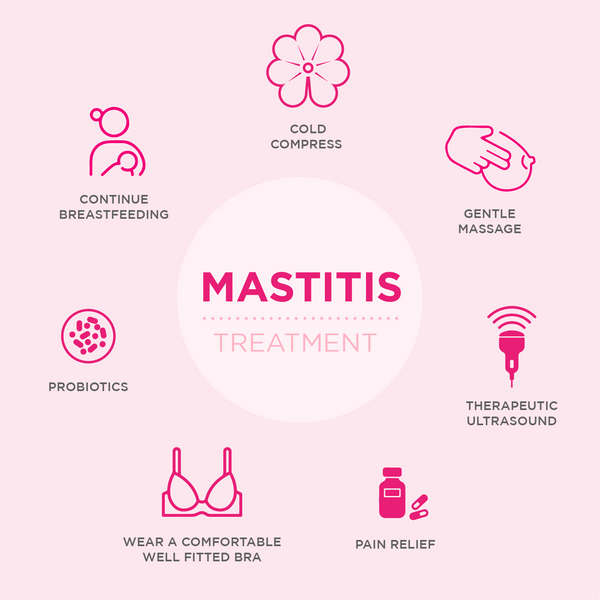
Pain Relief:
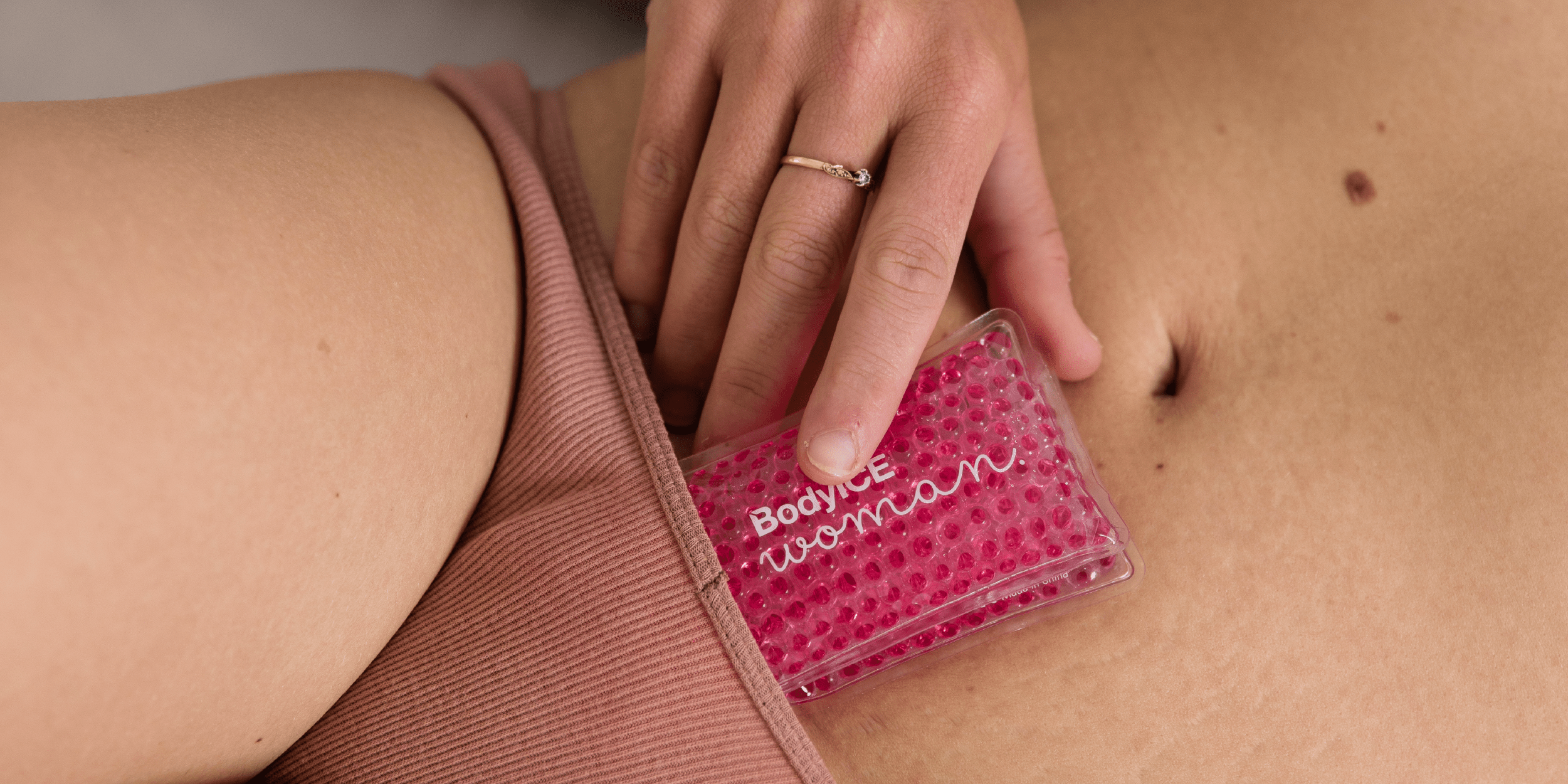
Icing using BodyICE Woman Breast Ice Packs can reduce swelling and provide relief to the sore breast. It is important to note that using a heat pack may worsen symptoms, therefore using cold packs can be much more efficient in improving symptoms.
Over the counter medication such as ibuprofen and paracetamol can also help with pain relief and inflammation.

Ensure the breast is draining effectively:
Seeing a lactation consultant to check your baby's latched properly and effectively draining the breast is an important step in reducing the reoccurrence of mastitis.
Utilise therapeutic ultrasound:
Therapeutic ultrasound utilises thermal energy to reduce inflammation and relieve swelling. It can only be performed by a trained physiotherapist.
Antibiotic Treatment:
If the cause is a bacterial infection, antibiotics for mastitis are prescribed to eliminate the infection. It is important that the antibiotics are only used for bacterial mastitis to reduce the risk of developing resistant pathogens. It's important to complete the full course of antibiotic medication, even if symptoms improve.
Probiotics:
The breast microbiome, the community of microorganisms residing in breast tissue, can be disrupted in cases of mastitis, potentially contributing to the inflammation and discomfort experienced during this condition. There is some evidence to suggest that probiotics might be effective in the treatment and prevention of mastitis, but only those of the Ligilactobacillus salivarius strains.
Continued Breastfeeding:
Contrary to popular belief, continuing to breastfeed on the affected side is crucial. It helps drain the breast, clear the infection and prevent the breast milk becoming stagnant. It is completely safe to breastfeed your baby from this breast and they will not “catch” the infection. Continue to feed on alternate breasts, and minimise breast pump usage.
Rest and Hydration:
Adequate rest and staying well-hydrated can expedite the healing process and support the immune system.
Avoid:
Avoid deep massage and excessive pumping, as this can actually make the inflammation worse. Try gentle massage or manual lymphatic drainage, which you can do by lightly sweeping up from the nipple towards the armpit.
Preventive Measures:

There are a few ways that you can try to prevent the development of mastitis. These may include:
- Ensuring a proper latch to reduce any nipple damage and reduces the risk of infection.
- Regular breast emptying: Feeding your baby on demand and frequently can help the milk to continue moving through the breast and reduce the risk of it staying stagnant.Warm compresses before feeds can also assist in the milk flow.
- Comfortable breastfeeding bras: Wearing wirefree, comfortable (not tight) breastfeeding bras can make sure that the bra isn't cutting in and potentially blocking some of the milk ducts. Also try to air out the breast between feeds.
- Maintaining good hygiene: Always wash your hands before and after touching your breasts. Use silver nipple cups early if you have any damage and make sure to clean these adequately in between use. Also make sure you change your breast pads frequently (check out our BodyICE Woman reusable nursing pads for an eco-friendly and comfortable option), and nipple shields may help if you are suffering from sore or damaged nipples.
When to Seek Medical Help?
While mild cases of mastitis should improve with home care, it's important to seek help from your health care professionals if symptoms worsen or if there's no improvement.
Mastitis is a common condition that significantly impacts families and women's decisions to continue breastfeeding. By understanding its causes, recognizing its symptoms, and adopting preventive measures, individuals can effectively manage mastitis and minimise discomfort. Early intervention and proper care can lead to a quicker recovery, allowing breastfeeding mothers to continue without major interruptions. Remember, seeking medical advice when necessary is crucial to ensure the best outcome for both the individual and the baby.
Written by Lauren Brenton - Founder of One Mama Midwife Pty Ltd.




Leave a comment
All comments are moderated before being published.
This site is protected by hCaptcha and the hCaptcha Privacy Policy and Terms of Service apply.